The Power of Being Present: How Meditation Can Transform Your Mental & Physical Health

Meditation has been on the rise across social media and self-care centered media, for good reason. Studies have shown promising results for the mental health benefits of meditation, including reducing anxiety and mental stress levels. It should come as no surprise that many therapists incorporate meditation into their practices.
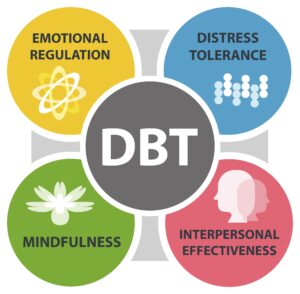
One popular form of therapy that has shown great success in reducing anxiety and depression symptoms, Dialectical Behavior Therapy (DBT), draws from Zen Buddhism and mindfulness, which both incorporate meditative practices. Keep reading to learn about the benefits of meditation and how to incorporate meditation into your mental healthcare and wellness routine.
Who can benefit from meditation?
You don’t have to be an expert or a guru to benefit from meditation. Along with the many benefits that meditation can bring you, it can be done by anyone, anywhere, at any time, for free! For those with anxiety disorders, such as Generalized Anxiety Disorder (GAD), meditation has been shown to be highly successful in improving symptoms, reducing anxiety and improving outcomes for those with this mental health disorder.
A blog post titled “Mindfulness meditation may ease anxiety, mental stress”, which was published on Harvard Health Publishing, Harvard Medical School’s blog, shared that Johns Hopkins University researchers reviewed close to 19,000 studies on meditation, finding that mindfulness meditation can be highly beneficial in regards to psychological stresses such anxiety, depression and pain. To learn more about these studies, click here.
The blog also shared similar findings from Dr. Elizabeth Hoge, who is a psychiatrist at the Center for Anxiety and Traumatic Stress Disorders at Massachusetts Hospital and an assistant professor of psychology at Harvard Medical School.
“If you have unproductive worries, you can train yourself to experience those thoughts completely differently,” says Dr. Hoge. “You might think ‘I’m late, I might lose my job if I don’t get there on time, and it will be a disaster!’ Mindfulness teaches you to recognize, ‘Oh, there’s that thought again. I’ve been here before. But it’s just that—a thought, and not a part of my core self.”

How can meditation benefit me?
Meditation can provide many benefits including physical, emotional and cognitive benefits.
An article by Headspace outlines the following 12 benefits of meditation:
- Reduced Stress
- Mindfulness Meditation in particular has been shown to reduce the inflammation caused by stress. This reduction in inflammation can both lower stress levels and improve physical conditions caused by stress.
- Decreased Anxiety Levels
- Since meditation can help lower stress levels, this results in reducing anxiety as well.
- Better Emotional Health
- Meditation can lead to an improved outlook on life and improved self-image due to a decrease in negative thoughts.
- Enhanced Self-Awareness
- Meditation teaches us to be present in our bodies and in our thoughts which can result in an enhanced understanding of ourselves.
- Improved Attention Span
- Since meditation is a focused practice, it can lead to an improved attention span.
- May Reduce Age-Related Memory Loss
- Studies have shown that meditation can actually improve performance on neuropsychological tests for those experiencing age-related memory loss.
- Increased Positivity & Kindness
- Certain forms of meditation include a special focus on generating positive feelings both towards yourself and others. According to Healthline, “Through practice participants can better learn how to extend kindness and forgiveness eternally, first through friends, then acquaintances, and ultimately enemies.”
- May Help Fight Addictions
- When meditation is used as part of treatment for substance use disorders such as alcohol use disorders, it can help participants develop mental discipline which can help them fight dependencies and triggers. Meditation can also help control food cravings.
- Improved Sleep
- In one study on insomnia/sleep disorders, meditation was shown to help participants stay asleep longer and improved their insomnia severity. This is likely because meditation can help relax your body, release tension and help fight against racing thoughts by bringing you back to the present moment.
- Reduced Physical Pain
- Some research has shown that meditation can improve the feeling of physical pain, since perception of pain is connected to your state of mind. The stress reduction aspect of meditation can be particularly helpful in improving stress related disorders such as irritable bowel syndrome (IBS), post-traumatic stress disorder (PTSD) and fibromyalgia.
- Can Decrease Blood Pressure
- Meditation can help control blood pressure by relaxing nerve signals which correlate with blood vessel tension, heart function and that can trigger the “flight or fight” response.
- Meditation is Accessible Anywhere!
- Meditation is a super inclusive practice that requires no special equipment or space. Meditation can be practiced no matter what age you are, and there are virtually limited guided meditations that are available for little to no cost.

Different types of meditation
When it comes to meditation practices, it isn’t one-shoe-fits-all. Fortunately there are many different types of meditation out there to explore.
5 Types of Meditation:
- Mindfulness Meditation
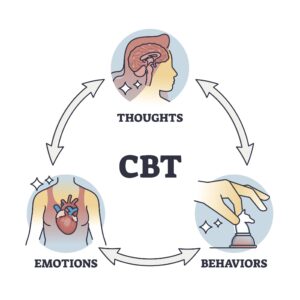
- Mindfulness meditation is often incorporated into Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT). The concept behind this type of meditation is rooted in mindfulness which is the practice of being fully present with yourself, your body, your thoughts and emotions in order to observe them without judgment.
- Guided Meditation
- In this form of meditation, a guide instructs you through relaxing certain muscles, controlling your breath, and visualizing mental images or concepts. This form of meditation can be especially helpful for those who are new to meditation.
- Loving-Kindness Meditation
- Also known as metta meditation, in loving-kindness meditation you direct loving energy and wishes towards both yourself and others. This practice can help with self-acceptance, our connection with others, and help us let go of rage/anger and practice forgiveness.
- Transcendental Meditation
- Transcendental meditation involves silently repeating positive words or a personal mantra in order to ease the mind and relax.
- Movement Meditation
- During movement meditation, you will engage in a physical (but relaxing) activity involving repetition. Examples of movement meditation include yoga and tai chi.
If you’ve never meditated before, it may feel odd at first, which is why we encourage you to keep practicing to achieve full benefits. We also encourage you to try different types of meditation to find the type that fits best with you and your goals!

How can I practice meditation?
For self-guided meditation, free resources and guided meditations are available online, including on YouTube. Although Headspace, a guided meditation app, is a paid subscription service, free trials are available for new Headspace members. Headspace also has a Youtube channel with some free meditations.
For those who would like additional support and guidance with meditation concepts, mindfulness, and other helpful practices, Valera Health offers multiple DBT Skills Groups for both adults and adolescents/teens. Many of our individual therapy providers also offer DBT and CBT therapy.
Please note that our DBT Skills Groups are currently only available for those residing in the state of New York, but we will be expanding our therapy groups to other Valera Health states in the future—stay tuned!
If you’d like to schedule a free consultation with a Health Connector to join individual or group therapy through Valera Health, click here.