Valera Health is Here to Help Your Child or Teen with Their Mental Health

Emotional and mental health plays a pivotal role in developmental milestones for children and teens. If you’ve noticed your child, teenager or adolescent is struggling emotionally or behaviorally, Valera Health can help.
Our therapists, nurse practitioners and psychiatrists are highly experienced with working with children, teens and adolescents ages 6-17 and use a science-backed and age-appropriate approach to telemental healthcare.
Valera Health’s Child & Adolescent Program (CAP)
Valera Health’s licensed therapists, psychiatrists and nurse practitioners use data-driven treatment methods tailored to the individual needs of each child, teen or adolescent. Our providers work around you and your child’s schedule by offering flexible sessions that range from 30-45 minutes to accommodate after school needs.
Our providers have a proven track record of improving outcomes for Child and Adolescent Program (CAP) patients.
According to recent statistics, Valera Health’s CAP outcomes have shown an average decrease of 4.9 points from the baseline score (based on intake) for GAD screenings (standard screening model for Generalized Anxiety Disorder). PHQ scores (a.k.a. Patient Health Questionnaire) decreased 4.8 points from baseline on average.
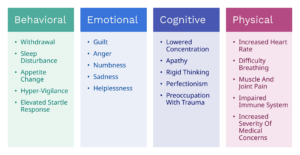
Our CAP providers specialize in helping children and teens with bullying, anxiety, depression, ADHD, school stress, grief and loss, childhood trauma, childhood mood disorders, behavioral issues, parenting issues, family/parental issues, anger management, self-harm and stress management.
We walk parents and caregivers through every step of their child’s treatment plan, so they can rest assured their child receives the high-quality care they need and deserve. Additional parental and/or familial support is also available as needed.

CHILDREN
Our CAP practitioners are highly-trained in age-appropriate mental healthcare for kids exhibiting signs of mental health issues. Our complete care model has been shown to be highly effective when it comes to treating common childhood difficulties such as anxiety, mood fluctuations, ADHD, school or family stress, adjustment issues and more. We offer treatment for children ages 6+.
TEENS & ADOLESCENTS
We offer a wide-array of specialized therapeutic and psychiatric services to help teens and adolescents adapt to challenges such as anxiety, depression, identity, trauma, confidence-building, stress management and much more. Our CAP providers understand how to connect with teens on both an individual and age-appropriate level. Teen and adolescent services are available for patients ages 13-17.
FAMILY + PARENTAL CARE
Parents and caregivers play a pivotal role in their children’s mental health—which is why we include them in their children’s wellness journey every step of the way. Providers meet periodically with parents to review their children’s progress through measured results. When appropriate, therapists may also meet with parents to review individualized parenting and communication strategies. We also provide individualized adult care for parents, families and caregivers to help them face familial and parenting/caregiving challenges head on.

How Do I Get Started?
We make finding mental health support for your family easy with our simple consultation and matching process. The first step is to submit an online consultation form to let us know what services you’re looking for. After you’ve submitted your consultation form, a Health Connector will help you find a provider who is a perfect fit for your child, adolescent or teen. From there, you can expect individual intake meetings for both yourself and your child with your chosen provider(s).
Parents/caregivers will be included in their child’s ongoing care and communications so they will always be in the know.
Get started today by clicking here or visiting www.valerahealth.com/consult-today/ to schedule a free consultation!