4 Ways Talk Therapy Can Help You

A common misconception about therapy is that you have to be seriously ill to benefit from it, or that it simply doesn’t work. The statistics, however, say otherwise—research has shown that roughly 75% of people who participate in talk therapy find it to be beneficial, according to the American Psychological Association.
No matter what challenges life throws our way, therapy can benefit anyone.

4 Benefits of Talk Therapy
1. Long-Lasting Results
Therapy provides patients with tools that they can take with them throughout the rest of their lives to healthily work through and cope with future problems.
2. Improved Physical Health
Mental health and physical health go hand in hand. Research suggests there is a strong correlation between poor mental health and poor physical health. Certain mental health conditions such as depression can cause or worsen physical ailments including digestive issues, bad sleep, immune system problems and more. So, it only makes sense that working through psychological issues and improving our mental health could result in improved physical health.
3. Repressed Emotions Don’t Always Stay Repressed
While some people think repressing their emotions means they don’t have to deal with them, this usually backfires. Repressed emotions can come out at any time, and with a vengeance. Repressed emotions have been linked to depression, high blood pressure, heart disease, digestive problems, infections and pain. Repressing your emotions may also cause challenges when dealing with conflict and can make it difficult to connect with others. Therapy provides a safe space to work with a professional to deal with repressed emotions in a healthy way.
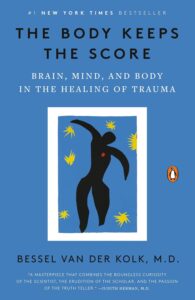
4. Rewiring Your Brain
Therapy can actually help rewire your brain for the better. One particular form of talk therapy known as Cognitive Behavioral Therapy (CBT) has shown great success at helping people identify habitual negative thought patterns and replacing them with positive mental habits. Check out this scientific journal article to learn more about the positive cognitive effects of CBT.

In-Person Therapy VS. Online Therapy
Both in-person and virtual therapy can result in equally positive patient outcomes. In fact, studies have shown that online therapy is just as effective as in-person therapy.
One benefit of online therapy over in-person therapy is that sessions can take place from virtually anywhere. Other benefits of remote therapy include its affordability, flexibility and that it can be done from the comfort of your own home. Check out this blog post to learn more about the benefits of online therapy.
If you’re interested in online therapy, click here or visit https://www.valerahealth.com/consult-today/ to request a free consultation with a dedicated Health Connector who will match you with a provider who’s tailor-made for you. In addition to individual therapy, we also offer virtual group therapy, psychiatry, medication management and more. Click here to learn more about our services and to get started on your wellness journey.