Reset Your Routine With These Positive Daily Habits

Amongst the chaos of our everyday lives, it’s easy to develop bad habits or throw good ones out the window before we know it. By pausing and creating an intentional daily routine, we can combat the chaos and live happier, healthier and more fulfilling lives. That’s why we created this list of healthy habits that can easily be incorporated into every daily routine. Keep reading to learn more.

Sleep Well
Technically, this part of a daily routine starts the night before—but that’s because good sleep plays a fundamental role in any health-conscious daily routine. A good night’s rest can kick-start a successful day by reducing stress levels, improving mood, increasing energy levels, decreasing anxiety and improving focus and memory. Aim for 7-9 hours of sleep per night—the doctor recommended amount.
7 Tips for Better Sleep:
- Go to bed and wake up at the same time each day and night, even on the weekends.
- Avoid screens at least an hour before bedtime.
- Limit caffeine and alcohol consumption—and don’t drink either for at least a couple of hours before going to bed.
- Read a book, drink a cup of non-caffeinated herbal tea (try one of these bedtime teas) or take a bubble bath to promote relaxation and send signals to your body and brain that it’s time to go into sleep mode.
- Invest in a comfy bed and pillow/sheet set and wash your sheets regularly.
- Sleep in a dark and cool environment with a temperature around 65°F.
- Use a sleeping mask and earplugs to limit exposure to light and noise while you rest.

Come Prepared
Prepare for the day ahead of you the night before so you don’t have to rush in the morning. Here’s how to do it: make breakfast or lunch the evening before. Pick out your clothes for the next day so you don’t have to spend time thinking of what to wear in the morning.
Wake Up with Intention
After you wake up and before getting ready, set a simple intention and affirmation for the day. Here are some examples of daily intentions to get you started: “Today, I will practice gratitude,” “Today, I will focus on the positives,” and “Today, I will be kind to myself and to others.”
After deciding on a daily intention, choose an affirmation, which is a positive statement used to boost self-esteem. Some favorite affirmations include: “I am worthy,” “I am strong,” and “I am right where I’m supposed to be.”
Keep a journal by your bed so you can easily write down your daily intention and affirmation first-thing in the morning.
Write It Down
Either the night before or in the morning—but before you dive straight into work—write down a to-do list of all the things you need or want to accomplish that day. This should include both work tasks and personal tasks.

Eat a Nutritious Breakfast
As the saying goes, “Breakfast is the most important meal of the day.” A healthy breakfast can give us the energy we need to take on the day, while also boosting our mental health and focus. Some easy, delicious and nutritious breakfast foods to try are fruit (such as bananas or berries), oatmeal or overnight oats, eggs and yogurt. Homemade smoothies are another great way to get essential nutrients on the go.
Stay Hydrated
Drinking water throughout the day not only helps with energy, but also helps with cognitive functioning. Start your morning off by drinking a glass of water, and keep a large reusable water bottle with you throughout the day. Make it a goal to drink the recommended daily water intake every day, which is 15.5 cups (3.7 liters) of water for men and 11.5 cups (2.7 liters) for women.

Practice Morning Meditation
Meditation has many positive benefits for both our physical and mental wellbeing.
Some of these benefits include:
- Reduced stress
- Decreased anxiety levels
- Better emotional health
- Enhanced self-awareness
- Improved attention span
- Increased positivity + kindness
- Improved sleep
- Reduced physical pain
- Decreased blood pressure
Even 5-10 minutes of morning meditation can provide positive mental health benefits. Check out this blog post to learn more about different types of meditation and ways to practice.
Set Aside Time for Self-Care
Make sure to schedule some “me time” every day. Use your designated “me time” as an opportunity to rest, unwind and reconnect with yourself.
Here are some ways to practice “me time”:
- Take a coffee or tea break outside. Drink your beverage slowly and take time to really enjoy each sip, breathe fresh air and watch your surroundings.
- Read a good book.
- Have a dance party with yourself.
- Watch an episode of your favorite show.
- Take a nap.
- Paint or make a craft.
- Journal your feelings.
Whatever you do with your “me time,” it should be centered around self-care. For additional ways to practice self-care, click here.

Final Thoughts
In order to successfully change our routines and form healthy habits, it’s best to add one or two new practices at a time. As these become second nature, gradually add more healthy habits to your routine and do regular self check-ins where you can reflect on the impact and success of these new habits.
By slowly incorporating positive habits into our daily routines, we can drastically improve the quality of our lives, leading to positive, long-term change.
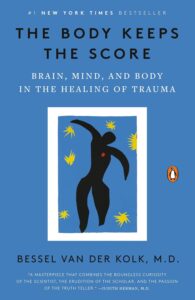
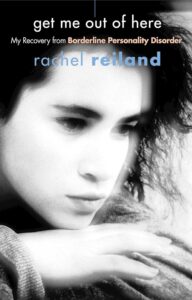
For more support with developing and sticking to healthy habits and improving your mental wellbeing, therapy is a great option. At Valera Health, we offer virtual individual therapy, group therapy, psychiatry and medication management so you can receive the care you need from the comfort of your own home. To request a free consultation with a Health Connector who will match you with a provider, click here or visit www.valerahealth.com/consult-today/.