We Need to Talk About the Children’s Mental Health Crisis

Childhood is a time full of learning and reaching developmental milestones that shape who we will grow up to be. Oftentimes, childhood is seen by adults through rose colored glasses—marked by nostalgia and fond memories. But this isn’t always reality.
Depending on many factors including one’s upbringing, social and educational experiences, genetics, health and more, childhood can be a tumultuous time full of change.
We tend to think of things such as depression, anxiety and stress as adult-only issues, but these things can affect children’s mental health and development in a multitude of ways.
That’s why we need to have candid discussions around children’s mental health and how we can support children who are struggling.

What Being Mentally Healthy Looks Like in Children
According to the Centers for Disease Control and Prevention (CDC), “Being mentally healthy during childhood means reaching developmental and emotional milestones and learning healthy social skills and how to cope when there are problems. Mentally healthy children have a positive quality of life and can function well at home, in school, and in their communities.”
Mental health plays a key role in the wellbeing of our children, and children who experience mental health issues and don’t get the help they need are more likely to experience additional difficulties down the road.
“Mental disorders are chronic health conditions—conditions that last a long time and often don’t go away completely—that can continue through the lifespan,” says the CDC.
“Without early diagnosis and treatment, children with mental disorders can have problems at home, in school, and in forming friendships. Mental disorders can also interfere with a child’s healthy development, causing problems that can continue into adulthood.”
Even if a child doesn’t qualify for a diagnosable mental health disorder, that doesn’t necessarily mean they are doing okay when it comes to their mental health.
As explained by the CDC, “Children who don’t have a mental disorder might differ in how well they are doing, and children who have the same diagnosed mental disorder might differ in their strengths and weaknesses in how they are developing and coping, and in their quality of life. Mental health as a continuum and the identification of specific mental disorders are both ways to understand how well children are doing.”
Warning Signs of Mental Illness in Children
How can we know when our child is having mental health issues? While they might not yet have the vocabulary or understanding of mental health to be able to tell us they are struggling, there are many ways children show they are having a hard time through their behaviors.
Signs to look out for include:
- Outbursts, tantrums or lashing out
- Extreme anger, rage or irritability
- Persistent sadness lasting two or more weeks
- Hurting oneself or expressing a desire to hurt oneself
- Fascination with death or suicide
- Hitting or acting violently towards other children or adults
- Drastic changes in mood or personality
- Sleeping problems
- Loss of weight or refusal to eat
- Frequent stomach aches
- Frequent headaches
- Extreme shyness
- Poor academic performance
- Difficulty focusing
- Avoiding or missing school
- Bullying others
- Reporting being bullied
- Being socially withdrawn or avoidant
Common Childhood Mental Health & Developmental Disorders Include:
- Anxiety Disorders
- Depression
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorder (ASD)
- Eating Disorders
- Post-traumatic Stress Disorder (PTSD)

The State of Children’s Mental Health By The Numbers
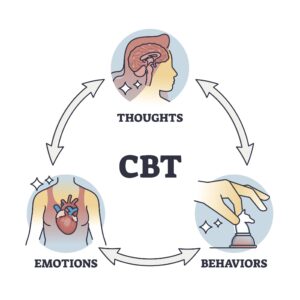
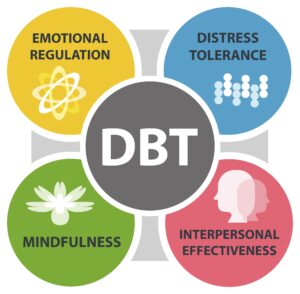
Oftentimes, anxiety and depression disorders are co-occurring, and various approaches to psychotherapy have been developed to treat them both. Among the most popular types of therapy for treating both anxiety disorders and depressive disorders are cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT), which are considered to be “gold standards” among psychologists.
Mental health disorders and struggles have no minimum age requirement, and impact more children than you might think. It’s estimated that 20 million of youth in the U.S. could currently be diagnosed with a mental health disorder (American Psychological Association).
According to 2023 numbers by Mental Health America (MHA), over 2.7 youth are currently experiencing severe major depression, with depression numbers found the highest in youth that are more than one race. In addition, 6.34% of youth were reported to have a substance use disorder, and 59.8% of youth with major depressive disorder (MDD) did not receive any mental health treatment this past year.
The same report shows that states with higher access to mental healthcare for youth have the lowest prevalence of mental illness in children than those without.
With mental health issues on the rise for America’s youth, providing proper resources and removing the stigma around children’s mental health plays a crucial role in combating the country’s mental health crisis.

How to Help if Your Child is Struggling
Many parents are hesitant to seek help for their children due to fear of being judged or labeled as “bad parents.” However, this couldn’t be further from the truth. Taking your child to a mental healthcare professional when they are struggling is no different from taking them to the doctor if they were sick with a bad fever or had a broken arm. Mental healthcare is the same as any other form of healthcare, and it shouldn’t be taboo. As parents and caregivers, it’s our responsibility to take care of our children when they are unwell.
From psychiatry and medication management to therapy, Valera Health offers specialized mental healthcare services for youth ages 6+ through its Child and Adolescent Program (CAP).
CAP is an inclusive, virtual mental health clinic rooted in evidence-based care for children and teens that also includes parental and familial support.
As an expansion to our CAP program, we are happy to announce that we are now offering group therapy programs designed for teens that are based in cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT). Valera Health has also launched a Conscious Parenting Group to help parents and caregivers navigate with the challenges that come with raising children, while also providing them with a safe space to connect with other parents.
Please note that currently these groups are only available to those who reside in the state of New York.
To learn more about individual therapy options for youth and parents, as well as our group therapy offerings, visit https://www.valerahealth.com/consult/ or click here.