The 7 Pillars of Self-Care

Self-care isn’t selfish. In our busy lives and fast-paced world, it’s easy to get stuck in our routines and a seemingly endless cycle of responsibilities, obligations and the stress that comes with it. We often tell ourselves, “Tomorrow I’ll take the time to do this,” or “This new habit starts next week,” and put the needs of others before our own. Whether it’s with work, our family, or our friends, we often neglect our own wellbeing in the process. Amidst the chaos of our daily lives, one crucial practice stands true for preservation: self-care!

What is Self-Care?
Self-care is more than just a buzzword—it’s a commitment to yourself to prioritize your mental, physical, and emotional health. Self-care is the deliberate actions one practices and incorporates into their life to help them to relax, unwind and maintain balance. According to the International Self-Care Foundation, there are seven main pillars of self-care that should be a part of every self-care routine.
What are the Seven Pillars of Self-Care?
Pillar #1: Knowledge and Health Literacy
The pillar of Knowledge and Health Literacy refers to an individual’s capacity to comprehend and grasp their own mental health and wellbeing. More precisely, it’s the knowledge that entails our ability to understand the body, what is good for it and how to nourish it. Another key element is access to resources that explain health conditions so that we can make smart and well-informed choices pertaining to our own health. Health literacy, in turn, encapsulates the manner in which people comprehend and assimilate health related information.
Pillar #2: Mental Wellbeing, Self-Awareness and Agency
Pillar two focuses on three main puzzle pieces that work together to create an essential part of self-care. Mental wellbeing emphasizes the importance of optimism, self-esteem and life satisfaction. Self-awareness highlights the everyday application of health literacy to evaluate how we feel mentally. Agency means calling attention to an individual’s commitment and intent to take action for their physical, mental and emotional health.
Pillar #3: Physical Activity
Physical activity is exactly what it sounds like! It’s any bodily movement that requires energy expenditure. Physical activity has so many benefits beyond looking and feeling good. It has the power to improve mental health. It contributes to better sleep, reduces stress, and can even help with self-esteem and building a stronger memory.
Pillar #4: Healthy Eating
Healthy eating sounds self-explanatory, but it’s more complex—and important—than you may think. Having a balanced and healthy diet helps build immunity, preventing disease and illness. Most importantly, the food you eat is what fuels you and helps you feel good throughout the day. Making sure all food groups are incorporated into your diet will help you feel better both mentally and physically, and can contribute to living longer.
Pillar #5: Risk Avoidance or Mitigation
Pillar five refers to the conscious caution and avoidance of behaviors or actions that are directly correlated with anything substantially dangerous, like getting a disease or, in some cases, death. Risk avoidance and mitigation highlight particular activities and due diligence that keep us safe and healthy. Some examples of this are drinking in moderation, taking medication only as prescribed, getting necessary vaccines on time, wearing a seatbelt, taking your daily vitamins and wearing SPF.
Pillar #6: Good Hygiene
When we first hear the word “hygiene,” what probably comes to mind is showering or brushing our teeth. In regards to pillar six, hygiene goes well beyond that. Hygiene in this instance refers to the circumstances and practices one initiates to keep steady with their health and preserve it. This can mean anything from drinking clean water to washing your hands in the effort to prevent disease. Good hygiene is a focal point in self-care. Access to proper sanitation and good hygienic practices are beneficial for not only our health, but well-being and economic productivity as well.
Pillar #7: Rational and Responsible Use of Products, Services, Diagnostics and Medicine
Pillar seven stresses the importance for individuals to make smart and informed choices when it comes to managing their health. This includes education about products and services, so that we can use medicine and other health products safely. It is the understanding of health services one may use like acupuncture, a trainer or a chiropractor. Acquiring the behind-the-scenes knowledge of risks and benefits of these products/services is crucial when it comes to making safe health decisions for ourselves.
How to Create Your Own Self-Care Routine
So, how do we implement these pillars into our everyday life? Though it can seem a bit daunting at first, the solution might be more simple than you may think: A routine!
Creating a personalized routine involves considering all of your individual needs in addition to the Seven Pillars of Self-Care. Self-care looks different from person-to-person and no two routines will look the same. Focus on what makes you feel centered, happy, and energized.
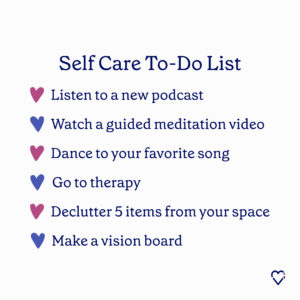
Here are some steps to get you started:
- Assess your needs. Reflect upon the current state of your emotional, physical and mental well-being. Try and identify areas which you think need a little more focus or nourishment.
- Find activities that rejuvenate you. Start by making a list of activities that you notice you feel your best while doing. This can be something big or small—from anything to listening to your favorite song or going for a hike.
- Prioritize these activities. Determine which of the activities you identified that align with what needs you want to work on and prioritize them.
- Establish a routine. Work on setting a designated time each day, week or month solely dedicated to self-care. Do it in regular intervals that work for you to create consistency. Treat this as a non-negotiable!
Start small, then grow. Begin by incorporating these activities in small intervals where they fit best. Over time, increase how much time you spend on these activities, and practice them regularly.
Additional Self-Care Resources
A huge aspect of self-care is allowing yourself to have a space to express your emotions and work through stressors.
Some people find this space to be an alone setting where they can enjoy their morning coffee with a book, while others find it more helpful to speak to a professional or connect with a group of others going through similar experiences.
Valera Health provides both individual and group therapy for those interested in therapeutic self-care.
At its core, therapy is a non-judgmental place that helps many work through large emotions that may be clogging up their minds. Therapy can help to understand and gain insight into these emotions. As we engage in therapy, we are engaging in the nourishment of prioritizing our mental health, honing in on pillar two of self-care. One of the very significant advantages of therapy, either in an individual or group setting, is the opportunity it presents to experience long-term mental wellbeing.
Along with one-on-one individual therapy, Valera Health offers many groups that support individuals at any point in their life, no matter what conditions they may be experiencing. From anxiety and depression, to parenting support, to a book club support group that was created as a cozy, supportive setting to gain knowledge through therapeutic literature and discussions, there’s a space for everyone at Valera Health. Call 646-450-7748 to schedule your first appointment.
For other resources check out the following:
- International Self Care Foundation (ISF): ISF is dedicated to sharing more about self care and what that means from individual to individual. Visit their website at http://isf-foundation.us/.
- American Psychological Association (APA): The APA has a designated page filled with all information about self- care and how to practice it in everyday life. Visit the website at: https://www.apa.org/topics/working-psychologist/self-care.

Works Referenced:
Burkett, M. (n.d.). The seven pillars of self-care. Recreation Services. https://recreation.ku.edu/seven-pillars-self-care
Iyarn. (2020, August 12). The seven pillars of self-care. https://iyarn.com/blog/the-seven-pillars-of-self-care/
Knowledge & Health Literacy – seven pillars – international self-care foundation. (n.d.). http://isf-foundation.us/index.php?m=content&c=index&a=show&catid=1&id=1
Lawler, M., Manning-Schaffel, V., Millard, E., Lucey, K., Dolan, M., Migala, J., Upham, B., Colino, S., Walsh, K., Lawler, M., & Byrne, C. (n.d.). What is self-care, and why is it so important for your health?. EverydayHealth.com. https://www.everydayhealth.com/self-care/
The seven pillars of self-care. ISF. (2020, July 20). https://isfglobal.org/practise-self-care/the-seven-pillars-of-self-care/
Transtrum, T. (2023, April 20). Why therapeutic self-care practices can lead to long-term wellbeing. Valera Health. https://www.valerahealth.com/why-therapeutic-self-care-practices-can-lead-to-long-term-wellbeing/
User, G. (2023, January 11). Understanding the 7 pillars of self-care. Mindful Maelstrom. https://www.mindfulmaelstrom.com/health-healing-resources-blog/understanding-the-7-pillars-of-self-care
What is self-care?. Global Self-Care Federation. (n.d.). https://www.selfcarefederation.org/what-is-self-care
Which kind of self-care do you need? take the self-care quiz!. The Blissful Mind. (2023, May 20). https://theblissfulmind.com/self-care-quiz/




















