By Grace Hickman, Laurie Engel and Taylor Transtrum

We often get mixed messages about alcohol. Advertisements, media depictions, and social practices normalize alcohol and make it look cool. Yet, despite the risks associated with alcohol use, alcohol is the most readily available substance out there, and the most socially acceptable substance to consume. Although alcohol consumption is so normalized, those with an alcohol use disorder are heavily stigmatized.
At Valera Health, we aim to take away the barriers that prevent people with an alcohol use disorder from getting help, while providing individualized care. Read on for signs you may have an alcohol use disorder, and ways Valera Health can help you.
For those who want to begin the healing process, group therapy is an excellent avenue on the road to recovery. Read on to learn more about what trauma group therapy is, its benefits, and how to join a trauma therapy group at Valera Health.

How Do I Know if I Have Issues Around Drinking?
Contradictory messages about alcohol use and alcohol use disorder can leave people unsure whether they have issues with alcohol use and if they should get help. While every person is different, if you identify with the bullet points below, we encourage you to consider seeking help.
Signs of Alcohol Use Disorder (AUD):
- You drink more than you mean to
- You want to stop drinking, but you can’t
- You’ve tried to stop drinking, but weren’t able to stop
- Drinking is taking over your life
- When you’re not drinking, you’re thinking about drinking
- Your drinking is getting in the way of your day-to-day activities
- Drinking is getting in the way of your relationships
- Drinking is getting in the way of work
- You find yourself doing risky things while drinking that you wouldn’t otherwise do when sober
- You know alcohol is bad for you, but you continue drinking anyway
- You need to drink more than you used to
- You experience withdrawal symptoms when you stop drinking
How Alcohol Can Affect Mental Health
Not only can alcohol use disorder cause physical issues, but it can put you at risk for severe mental health issues as well.
Excessive drinking has been shown to cause the following mental health issues:
- Depression: Alcohol can cause depression due to the chemical changes that occur in the brain when alcohol is consumed. Long-term alcohol abuse can lead to changing chemicals in the brain, which can cause feelings of sadness, hopelessness, and worthlessness.
- Anxiety: Alcohol can cause anxiety due to withdrawal symptoms that occur when an individual stops drinking. Individuals who are dependent on alcohol may experience panic attacks, trembling, and sweating when they attempt to quit drinking.
- Psychosis: While psychosis is often associated with other drugs, alcohol can cause psychosis as well. Psychosis, a mental health symptom characterized by losing touch with reality, can cause hallucinations, delusions and disordered thinking.
- Suicide: Alcohol can cause depression, hopelessness, and despair, which can lead to suicidal thoughts and actions.
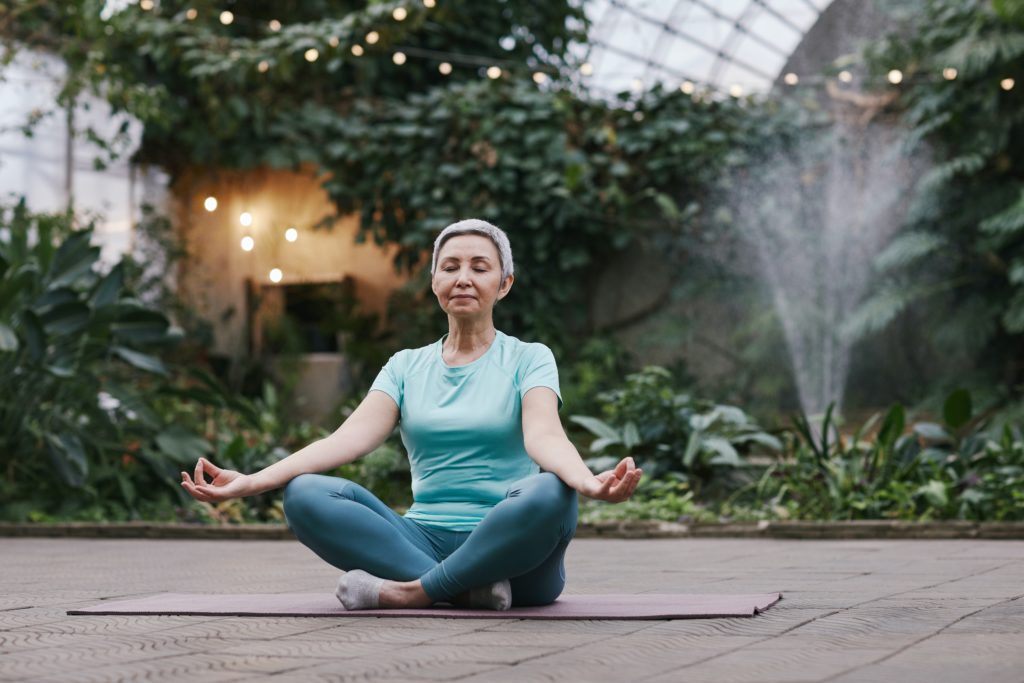
Mental health disorders can also result in alcohol use disorder as those suffering from these disorders tend to turn to alcohol as an unhealthy coping mechanism. Whether your alcohol use disorder is causing mental health issues, or preexisting mental health conditions are why you turn to alcohol, therapy can help you replace your alcohol use with healthy coping mechanisms.

Valera Health Can Help
At Valera Health, we have a specialized program to help patients who are dealing with co-occurring substance abuse disorders, such as alcohol use disorder, and other mental health disorders.
Valera Health’s Co-Occurring Disorders Program offers a combination of individual and group therapy, using interventions including Cognitive-Behavioral Therapy (CBT), and Motivational Interviewing. Motivational interviewing helps people overcome their fears or uncertainty, encouraging patients’ goal to get sober and begin their journey to recovery.
Please note, while our Co-Occurring Disorders Program tackles mental health and substance use disorders, it is not a substitute for detoxing off of alcohol or other substances.
Therapeutic Techniques Used to Treat Substance Abuse & Addiction
Group therapy has shown to be particularly effective in addressing problematic substance use. In a study on women with substance use disorders, researchers found that involvement not only improved outcomes immediately, but also six months after group therapy (Greenfield et al., 2014).
In addition to group therapy, motivational interviewing techniques have also been shown to be effective when addressing alcohol use disorder. In a study of individuals at a substance abuse treatment program, those who engaged in motivational interviewing therapy had less drinks and more days abstinent from drinking (Bein et al., 1993). Valera Health is pleased to offer a Motivational Interviewing Group as part of our Co-occurring Disorders Program, exclusively for patients experiencing substance use issues. In this group, clients will develop hope, confidence, and strengthen commitment.
Cognitive Behavioral Therapy (CBT), often referred to as the gold standard of therapy, has been shown to be effective in helping people with issues around substance use. CBT can help people struggling with alcohol addiction by teaching them to identify and monitor self-destructive thoughts and behaviors. Additionally, CBT can teach individuals to replace problematic thoughts and behaviors with more adaptive ways of thinking and skills for handling stress and difficulties. For example, in a study that examined the effectiveness of CBT among people experiencing substance abuse issues, 60% of participants remained sober for at least a year after the completion of therapy (Rawson et al., 2002).

How Do I Sign-Up for Therapy Through Valera Health?
At Valera Health we are invested in your recovery, and we have the resources to help you become the person you want to be. If you are interested in Valera Health’s services, please fill out this form to schedule a free consultation with a designated Health Connector.
Please note that at this current time, our virtual Co-Occurring Disorder Group is only available for established Valera Health patients who are located in New York. Stay tuned for more group therapy offerings from Valera Health in the future.
Works Referenced:
Bein, T., Miller, W., & Boroughs, J. (1993). Motivational Interviewing with Alcohol Outpatients. Behavioural and Cognitive Psychotherapy, 21(4), 347-356. doi:10.1017/S135246580001167X
Greenfield, S. F., Sugarman, D. E., Freid, C. M., Bailey, G. L., Crisafulli, M. A., Kaufman, J. S., … & Fitzmaurice, G. M. (2014). Group therapy for women with substance use disorders: Results from the Women’s Recovery Group Study. Drug and Alcohol Dependence, 142, 245-253.
Rawson RA, Huber A, McCann M, et al. A comparison of contingency management and cognitive-behavioral approaches during methadone maintenance treatment for cocaine dependence. Arch Gen Psychiatry. 2002;59(9):817-824. doi:10.1001/archpsyc.59.9.817
10 telltale signs that your drug use has gotten out of Control. Northpoint Washington. (2017, September 24). Retrieved March 29, 2023, from https://www.northpointwashington.com/blog/10-telltale-signs-drug-use-gotten-control/
What is Alcohol Awareness Month? Alcohol.org. (2023, January 19). Retrieved March 29, 2023, from https://alcohol.org/awareness-month/