Almost 70% of adults in the United States have experienced some sort of traumatic event at least once in their lives—but not all who experience trauma develop PTSD or C-PTSD.
Post Traumatic Stress Disorder (PTSD) and Complex-Post Traumatic Stress Disorder, C-PTSD, are two distinct psychological conditions that individuals who have experienced traumatic events can develop.
While these two conditions are related, it is important to recognize the notable differences in their underlying causes and symptomatology. Read on to learn more about these mental health conditions and what types of help are available.
Defining PTSD & C-PTSD
PTSD and C-PTSD are mental health conditions that can have a very profound impact on one’s daily life, relationships and overarching well-being.
Post Traumatic Stress Disorder (PTSD) is often a condition that is developed after a single traumatic event or incident. These incidents or events can include—but are not limited to—a sudden death, an act of violence, a natural disaster, being assaulted, or experiencing an accident.
C-PTSD, in turn, is referred to as “complex trauma” and it typically emerges from long-lasting exposure to trauma. Complex-PTSD is often framed in the context of experiencing abusive, neglectful or very stressful environments for a prolonged period of time.
While there are events that more commonly contribute to the development of PTSD and C-PTSD, it’s important to remember that all trauma is valid and you don’t have to experience a certain “type” of trauma to develop either of these conditions.

Signs & Symptoms of PTSD & C-PTSD
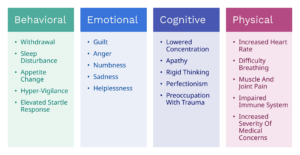
PTSD is a mental health condition that can manifest itself into many different and various forms of signs and symptoms following one’s exposure to a traumatic event. Understanding the signs and symptoms of PTSD is essential when recognizing the challenges one may face while living and working through this condition.
Signs & symptoms of PTSD may include, but are not limited to:
- Vivid flashbacks of the traumatic event, or feeling like you are reliving the moment the trauma first occurred
- Physical effects such as dizziness, chest pain, elevated heart rate
- Nightmares, especially if they are recurring
- Unable to express feelings or affection
- Avoidance of anything that may remind the individual of the event
- Feeling on edge, or experiencing severe anxiety
- Extreme alertness
Complex-PTSD can manifest itself in different ways that impact an individual’s life. When in a stressful environment for a long period of time, an individual may have a harder time recognizing signs and symptoms of C-PTSD.
While those with C-PTSD are also likely to experience the PTSD symptoms above, the key difference between the two disorders is that PTSD often occurs after a singular traumatic event, while C-PTSD can develop after experiencing chronic (long-term) trauma, or multiple traumas.
Additional signs and symptoms of C-PTSD may include the following:
- Feeling distrustful and hateful towards the world
- Feeling hopeless and as if there is no end to one’s suffering
- Feeling as though no one understands them or their trauma, or that no one can relate to what they are experiencing
- Experiencing dissociation, depersonalisation, or derealisation
- Thoughts of suicide
Please note that this is not an exhaustive list of all possible signs or symptoms of C-PTSD or PTSD. While most people with these disorders experience similar symptoms, C-PTSD or PTSD may look different from person-to-person.
If you or someone you know has experienced these signs or symptoms, we encourage you to speak to a licensed mental health professional, such as a therapist or a psychiatrist.
How PTSD & C-PTSD are Treated
When treating PTSD and C-PTSD, there are many different recommended interventions, but each and every person’s treatment journey is different depending on the individual and their needs.
One of the most common therapies used to treat PTSD is cognitive behavioral therapy (CBT). CBT aims to challenge the unhealthy thoughts that come with trauma and increase one’s emotional insight. Another therapy many providers try with patients looking to work through PTSD is prolonged exposure therapy. This approach helps individuals through gradually reprocessing repressed memories of the trauma they experienced in order to improve and build distress tolerance.
Eye movement desensitization and processing therapy (EMDR) is another popular form of therapy that can be highly beneficial for individuals with PTSD. Through EMDR, the individual reprocesses memories from the traumatic event with both guided instructions and rhythmic movements known as bilateral stimulation. Stimuli used in this treatment modality may include visual, auditory or tactile stimuli. Commonly repetitive and rapid eye movements are used as stimuli but tapping, tactile stimulation or auditory tones may also be used. The ultimate goal of EMDR is to give the individual the tools to no longer be distressed by memories of the traumatic event.
While the treatment of C-PTSD can be similar to the way PTSD is treated, there are a handful of additional therapies for individuals who have endured long-term trauma. Trauma focused cognitive behavioral therapy (TF-CBT) is often used for individuals who suffer with C-PTSD. This type of therapy helps individuals reframe their traumatic memories and overcome negative thoughts through developing effective coping skills.
Another kind of therapy recommended for those with C-PTSD is exposure therapy. Through exposure therapy, individuals are slowly encouraged to enter situations that make them uncomfortable or anxious and work through the situations to learn how to cope with the resulting feelings rather than suppressing or running away from them.
Group therapy is another kind of therapy that plays a crucial role in one’s treatment of PTSD or C-PTSD. A group therapy experience can allow an individual who may feel like they are not understood by anyone to connect with others who have endured similar traumas and provide them with a sense of validation and social support.
“It’s important that any treatment of trauma be through a trauma informed lens ensuring that the client feels safety, trust, collaboration, choice and empowerment and that the use of the therapeutic relationship be the cornerstone of treatment,” says Kelly Clark, who is Valera Health’s Clinical Lead for Trauma Informed Care.
How Valera Health Can Help
Valera Health provides telemental healthcare services tailored to meet the needs of any one with mental health disorders or related concerns. This includes trauma-informed care for those who suffer from conditions like PTSD and C-PTSD and anyone who has experienced trauma.

As part of Valera Health’s trauma-informed approach to mental healthcare, we have launched two group therapy programs designed to fit the unique needs of trauma survivors.
One of Valera Health’s providers who co-leads our Anxiety and Trauma Group, Abby Fink, shares the benefits of group therapy for those who have experienced trauma.
“Through group therapy, individuals within the group are able to offer each other a unique form of support that they may not receive from a one-on-one provider. Through the group experience, members are able to offer support to each other and gain a deeper level of understanding, empathy and, most importantly, validation.
C-PTSD, PTSD and trauma can lead many to feel isolated. Group therapy is an opportunity for individuals to connect with others who have also gone through similar struggles which can help reduce their sense of loneliness.”
Anxiety & Trauma Group: In this group, participants will find a space to discuss life transitions, school stress, and stress around relationships and decision-making. In this group, we will work together on developing coping skills to navigate daily stressors and other symptoms of anxiety. We will also explore how previous trauma impacts our daily functioning and impacts our goals in life.
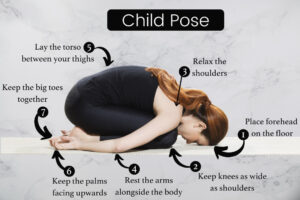
Trauma Survivor Group: Designed for young adults (ages 18-25), this trauma group teaches participants how to identify trauma responses as well as how to build coping skills for these responses. Participants will learn self-validation techniques, how to address triggers, grounding techniques for dissociation and fight-or-flight responses, how to reframe cognitive distortions and negative thoughts, basic self-care and mindfulness, the basics of journaling, how to discuss trauma with family and partners, and how to discuss relationship needs, boundaries and difficulties around sex.
This group is perfect for participants who are seeking a comfortable space where people share their trauma. This group was specifically designed for people who have experienced sexual trauma and/or relationship trauma.
To learn more about our virtual group therapy programs, click here. Please note, at this time our group therapy programs are only available for those residing in NY or MA, however we plan on expanding these services to more states in the future.
Valera Health also offers virtual one-on-one trauma-informed therapy for those who prefer individual therapy, as well as psychiatric services and medication management. If you are ready to start therapy, or are interested in learning more, call 646-450-7748 to speak with a Health Connector who will help you find the right treatment for you.
Whether you decide to go the group therapy route or prefer individual therapy, know that you have many options when it comes to your treatment.
Request a free consultation with us today to start your healing journey.
Additional Resources + Hotlines
National Alliance on Mental Illness (NAMI): NAMI offers information, support groups, and educational resources for individuals with PTSD and their families. Visit their website at www.nami.org.
National Institute of Mental Health (NIMH): NIMH provides comprehensive information on PTSD, including treatment options, research updates, and resources for finding mental health services. Explore their PTSD page at www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd.
PTSD United: PTSD United is an online community that offers support, information, and a platform for individuals with PTSD to connect and share their experiences. Find them at www.ptsdunited.org.
Works Cited
American Psychological Association. “Treatments for PTSD.” Https://Www.apa.org, June 2020, www.apa.org/ptsd-guideline/treatments.
“C-PTSD vs PTSD: Understanding the Differences.” Choosing Therapy, 21 Mar. 2022, www.choosingtherapy.com.
Child Welfare Information Gateway. Trauma-Focused Cognitive Behavioral Therapy for Children Affected by Sexual Abuse or Trauma. 2018.
“Complex PTSD.” Cleveland Clinic, 5 Apr. 2023, my.clevelandclinic.org/health/diseases/24881-cptsd-complex-ptsd.
“Free Photo | Eyes behind Broken Mirror.” Freepik, www.freepik.com/free-photo/eyes-broken-mirror_19002762.htm#query=trauma&position=0&from_view=search&track=sph. Accessed 9 June 2023.
“Free Photo | Young and Depressed Adult at Home.” Freepik, www.freepik.com/free-photo/young-depressed-adult-home_29973074.htm#query=ptsd&position=18&from_view=search&track=sph. Accessed 9 June 2023.
Mayo Clinic. “Post-Traumatic Stress Disorder (PTSD) – Symptoms and Causes.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 2018, www.mayoclinic.org/diseases-conditions/post-traumatic-stress-disorder/symptoms-causes/syc-20355967.
Mind. “Causes of PTSD.” Www.mind.org.uk, Jan. 2021, www.mind.org.uk/information-support/types-of-mental-health-problems/post-traumatic-stress-disorder-ptsd-and-complex-ptsd/causes/.
—. “What Is Complex PTSD?” Www.mind.org.uk, Jan. 2021, www.mind.org.uk/information-support/types-of-mental-health-problems/post-traumatic-stress-disorder-ptsd-and-complex-ptsd/complex-ptsd/.
The National Council for Mental Wellbeing. How to Manage Traum