As the sun goes down earlier and temperatures drop, we find ourselves longing for sunshine and warm weather. However, for some individuals, seasonal changes bring more than just a longing for summer again, and can cause the onset of seasonal affective disorder (SAD).
Seasonal affective disorder occurs in cases where “…these mood changes are more serious and can affect how a person feels, thinks and handles daily activities,” according to the National Institute of Mental Health (NIMH). SAD begins and ends around the same time each year, and typically resolves in the spring to summer months.
Fortunately, there are a handful of ways to relieve the symptoms of SAD that can be done from the comfort of your own home. You don’t have to wait until the warmer months come around to experience relief.
Tips for Coping with Seasonal Affective Disorder (SAD)
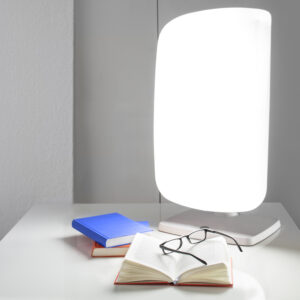
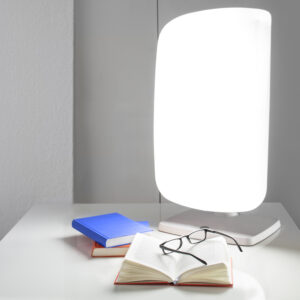
Tip #1: Get a light therapy lamp.
This type of lamp is specifically made to treat conditions like SAD. Because of the amount of light intensity they produce, light therapy lamps have the ability to mimic sunlight, which in return triggers positive mental and biological effects. Experts recommend that you should slowly ease into the use of your light therapy lamp, gradually leading up to using this light for about a half an hour per day. They also find it crucial to expose yourself to some light in the morning (before 10 a.m.) so depressive thoughts and effects subside early on.
Tip #2: Wake up & go to bed with a dawn simulator.
Dawn simulators—a.k.a. sunrise alarms—are alarm clocks designed to help you improve sleep by waking up and going to bed gradually. By using timed lights, they mimic how the sun rises in the morning and sets at night, tuning in with natural circadian rhythm patterns. Dawn simulators are known for benefits such as boosting energy, improving sleep and decreasing stress levels.
Tip #3: Exercise.
Exercise is one of the best ways to release feel-good endorphins—a fast acting mood booster. Exercise can help ease feelings of depression and anxiety. Getting enough exercise is also a great way to calm down and clear the mind. During winter and fall months, gyms provide a solid place to exercise without having to brave chilly weather. Or, if you prefer to stay in, these at-home exercises will get you moving.
Tip #4: Journal.
Journaling can help you release your thoughts and feelings, which in turn can help improve anxiety and mood levels. We recommend utilizing specialized journal prompts designed for those experiencing SAD in mind—one one of which can be downloaded here.
Tip #5: Limit alcohol consumption.
When you’re experiencing constant low moods, it can be easy to turn to alcohol for comfort. However, this is actually counterproductive as drinking when depressed can result in worsening depressive symptoms and spiraling negative thoughts. Although it may be tempting, It’s important to be conscientious of how much you’re drinking and how it makes you feel so you don’t end up feeling even worse—both physically and psychologically.
Tip #6: Aromatherapy.
Aromatherapy—or diffusing or rolling essential oils—is a great way to quickly boost your mood and promote relaxation. Putting essential oils in a diffuser or taking an aromatic bath before bed are great ways to channel inner peace and calm.
Aromatherapy experts recommend these oils for improving SAD symptoms:
- Patchouli Oil (Pogostemon cablin)
- Bergamot Oil (Citrus bergamia)
- Cardamom Oil (Elettaria cardamomum)
For more oils that promote relaxation and help with depression symptoms, click here.

Tip #7: Stick to a schedule.
Schedules are crucial when dealing with SAD, as many individuals with this condition struggle with waking up and sleeping. Being able to keep a steady and regular schedule is very helpful when it comes to improving sleep quality and keeping your body in a balanced state throughout the day. According to the Mayo Clinic, “Keeping a regular schedule will also expose you to light at consistent and predictable times…which is beneficial for your circadian rhythm.”
Tip #8: Consider medication.
Antidepressants can be a helpful tool for combatting the depressive symptoms that come with SAD. If you’re considering going on antidepressants for SAD, make sure to consult your doctor first.
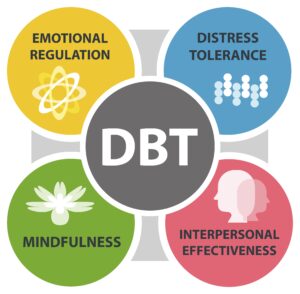
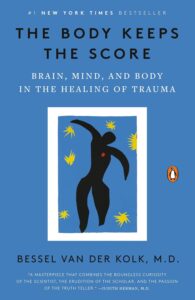
Tip #9: Try Therapy.
Therapy is a great way to learn coping strategies for managing and improving SAD symptoms. In therapy, you can learn new skills to help you navigate the emotional lows that come with SAD and receive much needed support during these difficult seasons.

Final Thoughts
At Valera Health, we offer virtual mental healthcare treatment tailored to each individual. Our services include individual therapy, group therapy, psychiatry and medication management—all of which can be effective tools for individuals with seasonal affective disorder. Our seasonal Holiday Support Group can help participants find relief and manage the unique struggles that come with this time of year such as SAD, stress, loneliness and more.
Whether you’re struggling with SAD or other mental health issues, we’re here to help you find the right provider for you. To request a free consultation with a Health Connector who can match you with a provider, visit https://www.valerahealth.com/consult-today/ or click here.
Remember that seasonal affective disorder is temporary. By practicing self-care and being aware of your needs and challenges around SAD, you can find relief.
Works Referenced:
Beth W. Orenstein and Michelle Pugle. (n.d.). 14 ways to ease seasonal depression. EverydayHealth.com. https://www.everydayhealth.com/depression/treatment/ways-to-ease-seasonal-depression/
Health, A. (2019, December 9). How to use light therapy for sad. Adventist Health. https://www.adventisthealth.org/blog/2019/december/feeling-sad-try-light-therapy/#:~:text=You%20should%20absorb%20light%20from,some%20light%20before%2010%20a.m.
Loeb, K. (2020, December 18). Tips for managing seasonal affective disorder (during a pandemic). Vail Health Foundation. https://vailhealthfoundation.org/news/tips-for-managing-seasonal-affective-disorder-during-a-pandemic/?gclid=CjwKCAjwp8OpBhAFEiwAG7NaEreVRwjA3xDEIhhywNhN17zDJylUEe0cWqy_Bt-vrHTHIrj77zeqVxoCdCYQAvD_BwE
Mayo Foundation for Medical Education and Research. (n.d.). Seasonal affective disorder (SAD). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/seasonal-affective-disorder/symptoms-causes/syc-20364651
Williams, K. (2023, October 7). 13 essential oils for seasonal affective disorder. Aromatics International. https://www.aromatics.com/blogs/wellness/13-essential-oils-for-seasonal-affective-disorde